Rural communities often face significant barriers to healthcare, including limited access to primary care, specialist services, and timely emergency interventions. The Mobile Integrated Healthcare Network (MIHN) exemplifies innovative strategies to bridge these gaps by delivering comprehensive, community-based medical services directly to patients’ homes. This approach not only enhances healthcare accessibility but also promotes patient engagement, improves health outcomes, and reduces overall healthcare costs. Understanding how MIHN functions and its impact can offer valuable insights into transforming rural health systems nationwide.
Overview
The primary goal of the MIHN, also known as the SHO-ME MIH Network in Missouri, is to bring preventive care and essential health services to individuals with chronic conditions living in rural areas. Many of these patients encounter obstacles in accessing traditional healthcare settings, leading to unmanaged health issues and frequent emergency visits. The program employs community paramedics (CPs) who conduct home visits, providing basic medical assessments, medication reconciliation, and facilitating telehealth consultations. This integrated approach ensures that patients receive timely, coordinated care tailored to their social and medical needs.
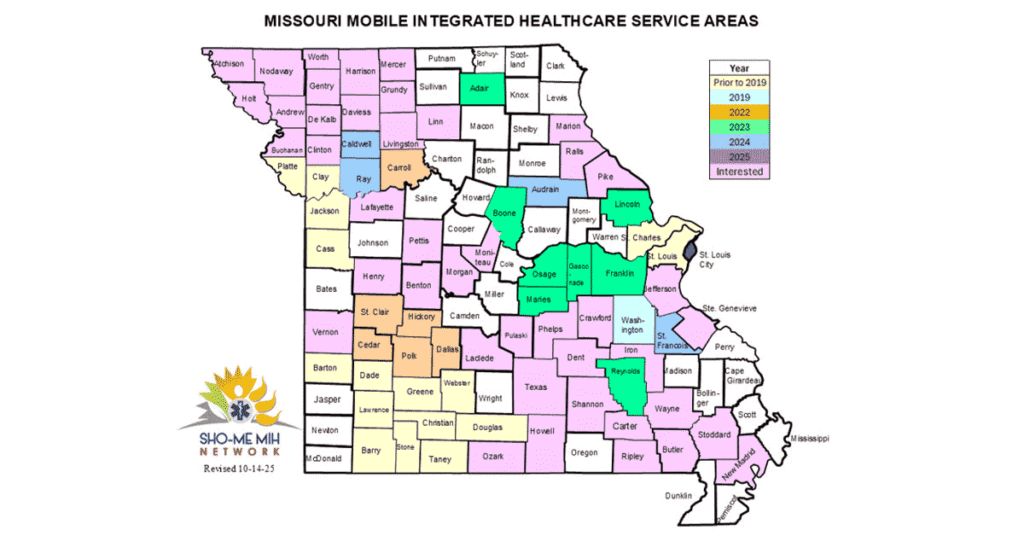
The program’s success can be partly attributed to its comprehensive service model, which emphasizes collaboration among healthcare providers, community organizations, and local government agencies. For example, partnerships with the Missouri Department of Health and Senior Services and the Missouri EMS Association enable continuous training and technical support for network staff. As the program expands across multiple counties in Missouri and neighboring Kansas, it demonstrates the potential for scalable rural health interventions that leverage existing community resources and federal funding.
In addition to managing chronic illnesses, MIHN has adapted to emerging public health challenges by offering COVID-19 testing, vaccination clinics, and food assistance programs. Recently, the network has expanded its scope to include substance use disorder services, such as field initiation of medication-assisted treatment like Suboxone, further addressing critical gaps in rural healthcare. For more on how to improve billing and reimbursement strategies for such complex services, see ways to enhance billing practices for shared healthcare.
Services Offered
Community health workers (CHWs) play a vital role in the MIHN by coordinating patient visits, assessing social determinants of health, and connecting individuals to local resources. During home visits, CPs provide a range of medical and supportive services, including:
- Conducting detailed health assessments, vital sign measurements, and lab sample collection
- Performing wound care and administering IV infusions
- Carrying out home safety evaluations to prevent accidents
- Reconciliation of medications to ensure compliance
- Facilitating telehealth sessions with healthcare providers
- Addressing social factors affecting health, such as food insecurity or housing issues
- Assisting patients with enrolling in primary care, Medicaid navigation, and care coordination
Patients can refer themselves or be referred by healthcare providers, emergency medical services (EMS), or hospital discharge teams. This flexible referral process ensures that high-risk patients who might otherwise fall through the cracks receive consistent, community-centered care. Integrating these services not only improves clinical outcomes but also reduces unnecessary emergency department visits and hospitalizations.
Program Results
The initial pilot in Washington County demonstrated remarkable improvements, with a 100% reduction in emergency transports among the 21 participating patients during the first year. The program facilitated approximately 7,000 encounters in 2021 and increased to around 8,000 in 2022, highlighting its scalability and community acceptance. These efforts significantly contributed to better management of chronic conditions, medication adherence, and overall patient well-being.
Currently, the SHO-ME MIH Network serves around 650 individuals across Washington, Reynolds, and Dent counties. Patients report enhanced access to healthcare services, improved health status, and greater engagement with community resources. Notably, the program’s cost-effectiveness is evident through analyses comparing expenses before and after enrollment, showing tangible savings for payers, hospitals, and community organizations. These savings are mainly achieved through reduced utilization of costly acute care services, demonstrating the economic value of proactive, community-based health interventions. For in-depth strategies on healthcare billing, refer to improving billing practices for complex healthcare services.
Challenges and Solutions
Implementing a rural mobile healthcare program presents unique challenges. One significant hurdle was limited internet connectivity, which impeded telehealth visits. To address this, program coordinators added mobile hotspots to MIHN vehicles, ensuring reliable communication and remote consultations. Additionally, the vehicles are equipped with refrigerators to transport blood and urine samples safely, maintaining sample integrity for laboratory testing.
Behavioral health needs also pose challenges, especially when patients exhibit resistance to care or struggles with behavioral health issues related to substance use. When non-compliance occurs, patients are linked to behavioral health specialists to determine if integrated mental health services are necessary, ensuring a holistic approach to their care.
Interesting:
- Advancing healthcare delivery through community paramedicine and mobile integrated health
- Unlocking healthcare efficiency through vertical integration
- Elevating healthcare customer service through effective training programs 2
- Elevating healthcare customer service through effective training programs
- Understanding united healthcare hearing your guide to hearing benefits and services
Workforce gaps emerged rapidly as service demand increased. To fill this gap, the program developed a pipeline of trained emergency medical technicians (EMTs), community health workers, and paramedics through partnerships with local community colleges. Scholarships and regional collaborations supported workforce development, ensuring a sustainable supply of qualified personnel. Funding remains a concern, but recent policy changes now allow Medicaid managed care organizations in Missouri to reimburse CP services via “in lieu of service” (ILOS) agreements, helping sustain program operations.
Data collection and monitoring posed significant obstacles initially. To improve this, the network partnered with a data platform capable of capturing and analyzing EMS and healthcare data in real time, enabling timely reporting and quality improvement initiatives. For more details on managing complex billing and data collection, see guidance on streamlining patient billing and insurance processes.
Replication and Future Directions
The MIHN model has been carefully documented, including workflows and best practices, to facilitate replication in other rural communities. Providing accessible tools and offering technical assistance helps other regions implement similar programs confidently. Building trust with patients is fundamental; dedicating time for conversations and addressing their questions fosters stronger relationships and enhances program success.
All CPs and EMTs involved in the network are certified as community health workers (CHWs), with some program pathways allowing students to earn both paramedic and CHW certifications simultaneously at institutions like Mineral Area College. This integrated training approach ensures a versatile, well-prepared workforce ready to serve rural populations effectively.
Contact Information
Justin Duncan, CEO
Washington County Ambulance District
—
This program exemplifies innovative rural healthcare delivery, combining mobile services, community engagement, and strategic partnerships. For further insights into rural health models and innovations, visit the Rural Health Information Hub.